Focus On COPD

The Global Initiative for Chronic Obstructive Lung Disease (GOLD)’s guidelines for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (COPD) are widely considered the go-to resource for treating patients with this condition. Test your knowledge of the 2018 version of the GOLD guidelines for COPD with this short quiz.
Understanding COPD
COPD has a dramatic impact on patients and public health. In the United States:
- 12 million people are currently diagnosed with COPD and an additional 12 million people with COPD have not received a diagnosis.1
- COPD and other lower respiratory diseases are the third leading cause of death.2
- Direct and indirect annual costs associated with COPD are estimated to exceed $50 billion.3
- Exacerbations of COPD cause more than 100,000 deaths and over 500,000 hospitalizations annually.4
- COPD is one of several diseases that has been identified for quality improvement efforts in health systems, and its management may affect payment models for providers.
Appropriate guideline-based selection and use of medications for the treatment of COPD can improve patient outcomes and quality of life as well as reduce the risk of exacerbations and hospitalizations.
Pharmacotherapy for COPD
Currently available medications used in the management of COPD do not change the progressive decline in lung function that is associated with the disease. Instead, the goals of pharmacotherapy for COPD include improving symptoms and decreasing exacerbations.
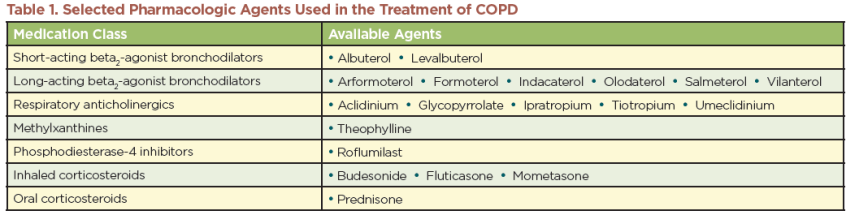
Several classes of medications are used to manage COPD (Table 1). Guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) provide recommendations for the treatment of COPD and include guidance regarding the role of each class of medication in therapy (http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd).5 According to these guidelines, medication selection is based on patient risks and symptom score, as measured by a validated assessment tool, and risk of future exacerbation, including frequency of exacerbations and hospitalizations:5
- Short-acting and long-acting bronchodilators are used for symptom management and include beta2-agonists and anticholinergics; methylxanthines are also part of this category but are used less frequently.
- Long-acting bronchodilators are also used to reduce exacerbations in patients at high risk.
- Corticosteroids control inflammation and are used primarily to improve symptoms and reduce exacerbations in patients at high risk.
- Phosphodiesterase-4 inhibitors are used to reduce exacerbations.
Most of these medications are delivered via inhaler and/or nebulizer. Theophylline and roflumilast are taken orally.
The Pharmacist’s Role in COPD Management
Pharmacists can help improve outcomes for patients with COPD through several strategies, including the following approaches:
- Develop and implement care plans to improve symptoms of COPD and prevent exacerbations.
- Educate patients about their medications and appropriate device use.
- Assess medication use and device technique at each subsequent visit to ensure the patient is using the device correctly.
- Provide ongoing support to address issues that may interfere with medication adherence, such as difficulties with inhaler devices, complex regimens, adverse effects, and cost.
- Assess each patient’s ability to recognize and act on symptoms of worsening disease.
- Support smoking cessation by providing smoking cessation services (e.g., counseling resources, nicotine replacement products, other pharmacotherapy) or directing patients to other available services.
- Offer vaccines that help prevent respiratory diseases, such as influenza and pneumococcal vaccines, as well as other appropriate vaccines.
- Support adherence to other individualized interventions, which may include oxygen therapy, adequate nutrition to avoid weight loss, pulmonary rehabilitation, or antibiotics.6
- Provide transitions of care services that support patients postdischarge and contribute to reducing the risk of readmission.
- Support access to care, including assisting the patient with navigating medication access barriers, recommending copay assistance programs and/or discount cards, and enrolling patients in manufacturers’ patient assistance programs, where applicable.
Patient Communication Strategies
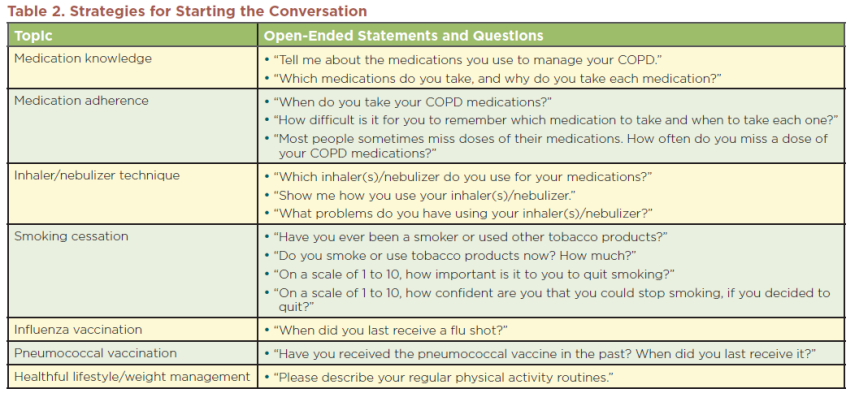
Patients require frequent and ongoing education about the management of COPD. Patient education should occur at diagnosis, during follow-up visits throughout the course of the disease, and when supporting patients during transitions of care. Pharmacists can ask patients open-ended questions to engage them regarding several topics that are important to the management of COPD (Table 2).
These questions are effective for eliciting information about the patient’s needs so that a plan can be developed to address those needs. Once education is provided to the patient, the “teach-back” technique is often helpful for ensuring that a patient understands the information. A good way to approach this is to say, “We just went over a lot of information and I want to make sure I didn’t forget to mention anything. Will you please explain what I said back to me?” Listen to the patient explain what he or she heard, and then clarify the information as needed.
The National Heart, Lung, and Blood Institute—part of the National Institutes of Health—provides materials to support the care of patients with COPD. These resources are available at https://www.nhlbi.nih.gov/health/educational/copd/campaign-materials/index.htm.
Strategies for Reducing Hospital Readmissions
Medication therapy management services designed to ensure patients understand which medications should be used when, and how to use those medications, are a key component of the treatment and management of COPD. Patients with COPD may be hospitalized for the treatment of exacerbations and they can experience high readmission rates. Reviewing the patient’s medication regimen and educating the patient and caregivers during transitions of care can not only
improve patient care but may reduce the risk of readmissions.7 Pharmacists can positively affect patient care throughout transitions of care by reviewing all aspects of the patient’s COPD management, ensuring that the patient is using appropriate medications correctly, and assessing and addressing other behaviors that impact COPD outcomes.
Medication reconciliation services designed to review a patient’s medication treatment regimen should be a key component of transition of care services. Such services are crucial for identifying and addressing adherence issues. Poor adherence has been associated with unnecessary escalation of therapy and reduced quality of life as well as increased morbidity, health care expenditures, hospitalizations, and possibly mortality.8 Medication adherence interventions should address both the medication regimen and the use of inhaler devices to support proper technique.
Device Education and Selection
Correct use of inhaler and nebulizer devices is crucial for the efficacy of inhaled medications. However, research indicates that up to 85% of patients use their inhalers for COPD ineffectively.9 Because of the importance of inhaler technique, regular evaluation of inhaler technique has been added to the recommendations in the GOLD 2017 guidelines. According to the guidelines, inhaler technique should be assessed at each visit to ensure the patient is able to use the inhaler correctly.
Pharmacists’ knowledge of correct inhaler and nebulizer technique, thorough patient education and demonstrations, and follow-up assessment skills are instrumental in optimizing device competency and medication adherence. Research has shown that patients’ inhaler technique improves following education from a pharmacist.10,11 Numerous educational tools are available to support efforts to train patients to correctly use their inhalers. For example, free training videos in multiple languages for over a dozen inhalers are available at http://use-inhalers.com. Many nebulizer manufacturers offer instructional videos; refer to specific device manuals for more information.
When selecting a device for medication delivery, there should be careful consideration of the needs, abilities, and limitations of the individual patient. Patients may be more likely to adhere to COPD therapy if their inhalers are simple to use and manage.12 This may be particularly true for older patients with COPD who have impaired physical and cognitive function that interferes with device adherence and proper use.13 If a patient is struggling with the use of their inhaler, the pharmacist may want to discuss options to switch to an alternate device (such as another inhaler or nebulizer).
Ideally, individual patients will be able to receive all inhaled medications via similar devices. Multiple inhaler devices that require different inhalational techniques may be confusing for the patient and result in administration errors. Additionally, switching among inhaler devices can have a negative impact on patient care if patients become confused about appropriate device technique.12 If a patient requires any medication changes that affect the type of device used to administer a medication, the pharmacist should assess the patient’s ability to use the new device and provide education about the new device.
Supporting Patient Access to Care
The cost of treatment is an important consideration that affects access to care. Formulary and coverage determinations, prior authorizations, and tiered copays are common practices for managing costs associated with some of the medications and devices used to treat COPD. Although such practices may control medication costs, they also may have a negative impact on patient care if they disrupt or delay patient access to medications and thereby interfere with patients’ ability to adhere to recommended pharmacologic therapy and maintain control of their COPD. Pharmacists can help address these barriers by working with patients and third-party payers to minimize medication access issues. Strategies include:
- Identify products that meet the patient’s medication needs and device needs.
- Evaluate the patient’s ability to access medications and help the patient navigate formularies to identify medications with a lower copay.
- Ensure that claims for devices are submitted separately when necessary.
- In some cases, devices must be reimbursed through a separate process from the medication reimbursement. For example, Medicare considers nebulizers to be durable medical equipment and reimburses these devices through Medicare Part B. More information about this process is available at https://www.cms.gov/Center/Provider-Type/Durable-Medical-Equipment-DME-Center.html.
- Identify programs that can assist patients with the financial burden of medications. For patients with no health care insurance, patient assistance programs sponsored by pharmaceutical companies can help to provide medications at reduced cost. For patients who have health care insurance but need assistance with copays, copay cards or copay assistance programs may be helpful.
- Copay cards are available to patients with commercial insurance plans, but they are not available for patients with federally funded insurance (Medicare, Medicaid, TriWest, VA benefits).
- Copay assistance programs are open to all patients, regardless of insurance status, but these programs are generally targeted at very high-cost medications and require forms to be completed by a physician.
- Information on medication assistance programs and other frequently asked questions can be found at http://rxassist.org.
Acknowledgments
The American Pharmacists Association (APhA) gratefully acknowledges the financial support from Mylan Specialty, LP, for the development of this resource, Focus on COPD: Pharmacists Helping Patients Improve Outcomes and Reduce Readmissions.
The following individuals served as APhA content developers and pharmacy practice advisors:
- Sharya Vaughan Bourdet, PharmD, BCPS
- Kelly Brock, PharmD
- Dennis Williams, PharmD, BCPS, AE-C
References
- National Heart, Lung, and Blood Institute. COPD Learn More Breathe Better. Available at: http://www.nhlbi.nih.gov/health/public/lung/copd/index.htm. Accessed October 30, 2017.
- Centers for Disease Control and Prevention. Leading Causes of Death. Available at: http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed October 30, 2017.
- Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235–45.
- Panettieri RA. Reducing Exacerbations in COPD. Available at: http://www.physiciansweekly.com/ reducing-exacerbations-in-copd. Accessed October 30, 2017.
- Global Initiative for Chronic Obstructive Lung Disease. GOLD 2017 Global Strategy for the Diagnosis, Management and Prevention of COPD. Available at: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prev…. Accessed October 12, 2017.
- Han MK. Patient education: chronic obstructive pulmonary disease (COPD) treatments (Beyond the Basics). Available at: http://www.uptodate.com/contents/chronic-obstructive-pulmonary-disease-…. Accessed October 30, 2017.
- Luder HR, Frede SM, Kirby JA, et al. TransitionRx: impact of community pharmacy postdischarge medication therapy management on hospital readmission rate. J Am Pharm Assoc. 2015;55:246–54.
- Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63:831–8.
- Restrepo RD, Alvarez MT, Wittnebel LD, et al. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–84.
- Barrons R, Pegram A, Borries A. Inhaler device selection: special considerations in elderly patients with chronic obstructive pulmonary disease. Am J Health System Pharm. 2011;68:1221–32.
- Hämmerlein A, Müller U, Schulz M. Pharmacist-led intervention study to improve inhalation technique in asthma and COPD patients. J Eval Clin Pract. 2011;17:61–70.
- Scichilone N, Benfante A, Bocchino M, et al. Which factors affect the choice of the inhaler in chronic obstructive respiratory diseases? Pulm Pharmacol Ther. 2015;31:63–7.
- Lareau SC, Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:401–6.
Disclaimer
Although every reasonable effort is made to present current and accurate information for public use, APhA and its employees and agents do not make any warranty, guarantee, or representation as to the accuracy or sufficiency of the information contained herein, and APhA assumes no responsibility in connection therewith. The information referenced in the document is provided “as is” with no warranties of any kind. APhA disclaims all liability of any kind arising out of the use of, or misuse of, the information contained and referenced in this document. The use of information in this document is strictly voluntary and at the user’s sole risk.

